So you've finally taken the plunge and gotten that bothersome mole removed. Whether you chose laser mole removal or surgical mole removal, the painful part is over and you're now faced with the recovery phase.
At this stage, you would be faced with damaged looking skin that slowly heals over. Even after the wound has healed over, the area may still look a little iffy, red or even depressed. Naturally, many patients worry that their mole removal would heal poorly, forming a scar.

Scars can be divided into two main types: atrophic or sunken scars, and hypertrophic/keloid or raised scars. Or it could just be that some blending is required to make the treated area more inconspicuous. When faced with a scary-looking wound, many patients would be very anxious to give their skin the best chance at a perfect scarless recovery and frantically search for solutions.

Don't freak out yet! Published research proves that some simple interventions improve the appearance of scarring after mole removal.
Topicals
Retinoids
Vitamin A derivatives such as tretinoin and adapalene enhance the wound healing process. They supercharge collagen production, ingrowth of new blood vessels and granulation tissue formation. I find them especially useful for deeper wounds that may otherwise end up as depressed scars. Retinoids also have beneficial effects on hypertrophic scars such as keloids.

Silicone
Silicone-based dressings favourably influence a wound’s electrical charge, promoting migration of new skin cells and allowing more rapid healing. Silicone products also reduce the risk of developing keloid/hypertrophic scars. I start almost all patients on silicone gel very early postoperatively.

Other topicals
Other treatments like platelet-rich plasma (PRP), growth factors like insulin, etc have also shown some positive effects in trials on wound healing.

Injectables
Polydeoxyribonucleotide (PDRN)
PDRN has long been used to improve wound healing, thanks to its ability to promote cell migration and growth, proper extracellular matrix deposition, generation of new blood supply and to reduce inflammation.
PDRN acts as a pro-drug capable to generate active deoxyribonucleotides, nucleosides, and bases. As a result, PDRN activates the salvage pathway and adenosine A2A receptors, widely known in the literature to blunt inflammatory responses and improve wound healing.
In my experience, PDRN really does improve wound healing, particular for deep and difficult wounds. However, it is quite pricey and thus I tend to use it for wounds that are at high risk of not healing properly.
.JPG)
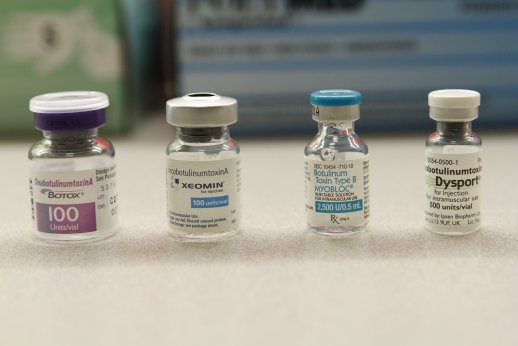
Neurotoxins
Neurotoxin-induced relaxation, known as “chemo-immobilization,” produces favourable results in the prevention of hypertrophic scars, improved wound healing, and amelioration of existing scars/keloids. Typically, I would use neurotoxin after mole removal via laser excision. This reduces pulling on the wound edges while the scar is strengthening, reducing the chance that the scar will widen. Sometimes I use neurotoxin for hypertrophic scars or keloids arising from mole removal wounds but those tend to be rare.
The good thing about neurotoxin is that it has a long duration of action and one injection can typically last for half a year by which time the scar would have significantly matured.
Lasers
Wound healing occurs through three phases: inflammatory (0–3 days), proliferative (4–21 days), and remodelling (22 days to 1 year or more). The traditional approach, to start laser intervention 3–6 months after, is way too late in my opinion. At this phase, the scar has already matured, fixed and difficult to convert to other tissues. My preference is to review all wounds early with a view to starting early laser therapy for the best final cosmetic outcome.
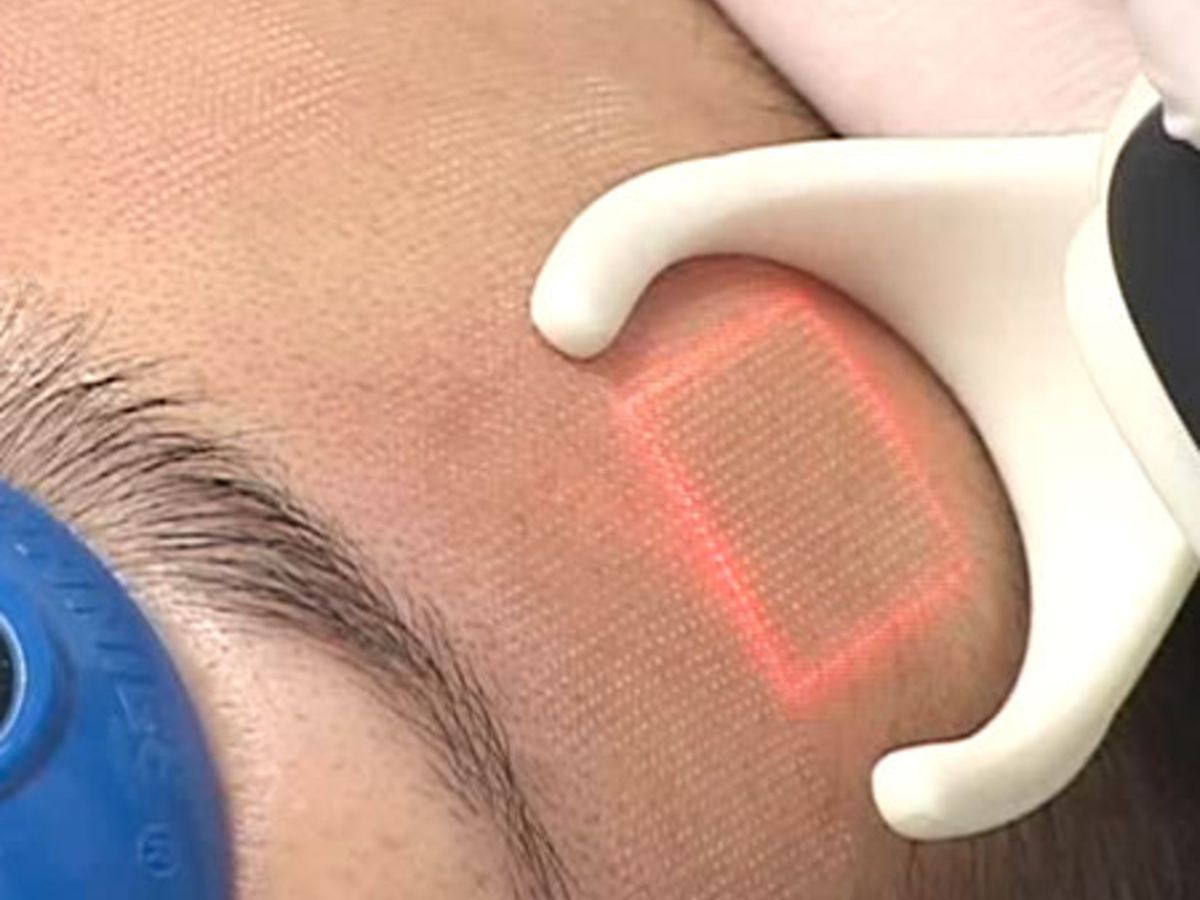
Fractional lasers
Fractional lasers such as CO2 or erbium lasers produce micro‐damage zones (MTZs) that trigger the wound healing process. This re‐orders disordered collagen, increasing the content of type III collagen, activating epidermal stem cells, reducing the amount of scar promoting factor transforming growth factor‐β1, and decreasing the number of local blood vessels.
I find fractional lasers effective for blending in scars to blur the boundary between the normal skin and the treated area. It is also useful for wounds that have healed but are still a little sunken, as it helps to stimulate more collagen to level out the sunken area. However, it has to be started early as the results are much better while the scar is still fresh.
Vascular lasers
Vascular lasers such as the gold, yellow or pulsed dye lasers are absorbed by the blood in blood vessels, leading to the destruction of abnormal vessels. Vascular laser applied to sutured wounds beginning at the time of suture removal normalizes tissue fibroblast density and collagen arrangement with lessened fibrosis and more elastin production. Vascular laser is particularly effective for hypertrophic or keloid scars, inducing regression and suppressing the over-active healing response.
I sometimes use vascular lasers as pre-treatment for keloid prone patients, but more often they are used to treat any raised scars that may develop. Personally, I find that vascular lasers work well for hypertrophic/keloid scars, particularly for early ones that are not too thick. Thick or mature keloid scars may need other treatments such as intralesional steroids or excision, hence it is important to monitor your mole removal healing and see your doctor early for review.

Conclusion
Aftercare, including blending with laser, peri-procedural neurotoxin, topical medications, is critical in achieving the best possible cosmetic outcome after mole removal. If you find that your mole removal wound is not healing well, see your doctor early so that we can intervene to enhance the final outcome. Many effective options exist and results are better if treatment is started early.
Do you have more questions about mole removal aftercare or worry about how your mole removal wound is healing? Please feel free to drop me a message!
References
- Abdelmalek M, Spencer J. Retinoids and wound healing. Dermatol Surg. 2006 Oct;32(10):1219-30.
- Basak PY, Eroglu E, Altuntas I, Agalar F, Basak K, Sutcu R. Comparison of the effects of tretinoin, adapalene and collagenase in an experimental model of wound healing. Eur J Dermatol 2002;12:145-8.
- Yong, A. A., & Goh, C. L. (2018). Use of silicone gel to enhance skin wound healing by secondary intention following tumour excision on the scalp and extremities. Clinical and Experimental Dermatology, 43(6), 723–725.
- Colangelo MT, Galli C, Guizzardi S. The effects of polydeoxyribonucleotide on wound healing and tissue regeneration: a systematic review of the literature. Regen Med. 2020 Aug 6.
- Guo X, Song G, Zhang D, Jin X. Efficacy of Botulinum Toxin Type A in Improving Scar Quality and Wound Healing: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Aesthet Surg J. 2020 Apr 14;40(5):NP273-NP285.
- Zhang Y, Liu Y, Cai B, Luo C, Li D, Wang S, Sun Z, Luo SK. Improvement of Surgical Scars by Early Intervention With Carbon Dioxide Fractional Laser. Lasers Surg Med. 2020 Feb;52(2):137-148.
- Kent RA, Shupp J, Fernandez S, Prindeze N, DeKlotz CMC. Effectiveness of Early Laser Treatment in Surgical Scar Minimization: A Systematic Review and Meta-analysis. Dermatol Surg. 2020 Mar;46(3):402-410.
